What’s new in breast cancer research? SABCS 2022 delivers plenty
Studies highlight research on treatment toxicity, disparities in insurance, gaps in metastatic care, new therapies and more.
Scientists and oncologists from around the world — including Fred Hutchinson Cancer Center in Seattle — shared a slew of new findings at the 45th annual meeting of the San Antonio Breast Cancer Symposium, held December 6-10 in San Antonio, Texas.
The largest scientific breast cancer conference on the planet, SABCS drew nearly 10,000 clinicians, researchers and patient advocates, with many attendees remaining masked due to ongoing COVID-19 and flu risk.
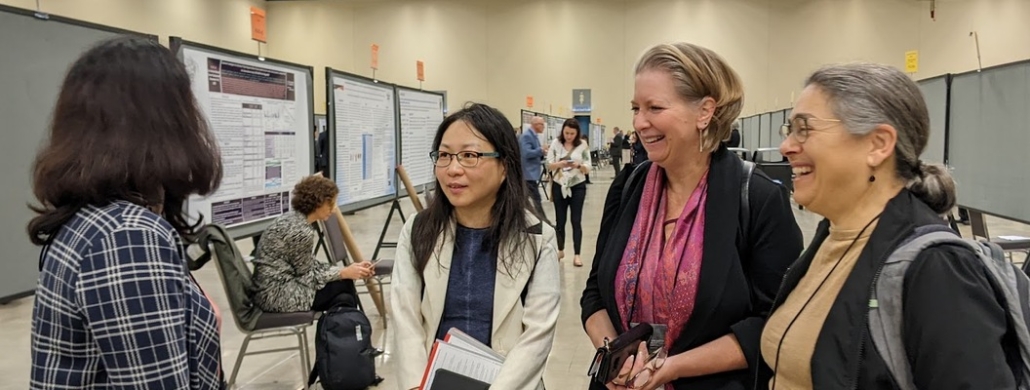
Fred Hutch breast cancer oncologists gather in the poster room at the San Antonio Breast Cancer Symposium, held in San Antonio, Texas, Dec 6-10. From left, Drs. Poorni Manohar, UNKNOWN, Jen Specht and Hannah Linden.
Photo courtesy of Diane Mapes
Scientists and oncologists from around the world — including Fred Hutchinson Cancer Center in Seattle — shared a slew of new findings at the 45th annual meeting of the San Antonio Breast Cancer Symposium, held December 6-10 in San Antonio, Texas.
The largest scientific breast cancer conference on the planet, SABCS drew nearly 10,000 clinicians, researchers and patient advocates, with many attendees remaining masked due to ongoing COVID-19 and flu risk.
Hot topics for the conference included results from large clinical trials including the POSITIVE trial, which showed taking a break from endocrine therapy for pregnancy did not impact short-term breast cancer outcomes (good news for young patients) and the TAM-01 or “Babytam” trial, which pointed to low-dose tamoxifen as a potential risk-reducing strategy for early, non-invasive breast cancers (think DCIS and LCIS) and a possible alternative for those who can’t tolerate the side effects of the usual 20-mg dose (although research on this is lacking).
Results from the ongoing DESTINY-01 trial were also announced, showing that the antibody drug conjugate, or ADC, trastuzumab deruxtecan (also known as T-DXd or Enhertu), demonstrated “clinically meaningful and statistically significant improvement” in overall survival of pretreated HER2-low metastatic breast cancer patients over another ADC, ado-trastuzumab emtansine (also known as T-DM1 or Kadcyla).
New antibody drug conjugates, along with CDK4/6 inhibitors, continued to show promise for patients, but most researchers agreed the drugs can have concerning side effects — which means clinicians need to be alert to the collateral damage of these targeted treatments.
“The rate of serious pulmonary toxicities such as interstitial lung disease [ILD] has gone down but it does raise the issue of safety,” said Fred Hutch breast cancer oncologist Jennifer Specht, MD. “As use of T-DXd extends to an even larger group of patients, we are reminded of the need for vigilance to identify rare and serious toxicities.”
Researchers from the Fred Hutch/University of Washington/Seattle Children’s Cancer Consortium presented findings in a number of areas, from data on new imaging tracers to analysis of treatment-related side effects like neuropathy to identifying gaps in metastatic cancer care. Read on for a few SABCS 2022 highlights.
Fred Hutch breast cancer oncologist and metastatic breast cancer researcher Dr. Kevin Cheung, chats with MBC patient advocate Christine Hodgdon, co-founder of GRASP (Guiding Researchers and Advocates to Scientific Partnerships) during the 2022 San Antonio Breast Cancer Symposium.
Photo courtesy of Diane Mapes
Assessing the collateral damage of treatment
Fred Hutch biostatistician and health services researcher Joe Unger, PhD was lead statistician on a study on peripheral neuropathy, a common side effect especially with taxane chemotherapies, that causes weakness, numbness and pain, usually in the hands and feet.
Commonly delivered by infusion, taxanes have been a cornerstone of cancer chemotherapy for decades; one type, Taxol, is the “best-selling cancer drug ever manufactured,” according to the National Cancer Institute’s Developmental Therapeutics Program timeline, with annual sales in 2000 reaching $1.6 billion. Projected sales for a new injection version of the drug are expected to reach over $11.16 billion by 2030.
But peripheral neuropathy continues to plague patients. How many suffer from this side effect?
Working with investigators from the SWOG Cancer Research Network, Unger analyzed data from an observational study that enrolled adults with early-stage non-small cell lung, breast or ovarian/fallopian tube cancer who’d started treatment with a taxane-based regimen and developed neuropathy.
The breast cancer group had approximately 1,200 patients, all of whom received either paclitaxel (Taxol) or docetaxel (Taxotere). Clinically meaningful sensory neuropathy was reported by 18.7% of the patients after just one month. By two months, 33% of patients reported neuropathy and by three months, the number of patients with neuropathy had grown to 46.3%. After six months, 44.8% of patients still reported neuropathy and a year later, nearly half of participants, 47.4%, had it.
“Altogether, over the entirety of the first year, two out of every three participants experienced clinically meaningful sensory neuropathy symptoms during treatment,” Unger noted, adding that given the high incidence, “it is critical to develop effective methods to predict, prevent and treat this toxicity.”
SWOG researchers also dug into data from their large international RxPONDER trial (launched to determine if certain early-stage patients can safely skip chemotherapy) to examine other common side effects of breast cancer treatment: cognitive impairment, fatigue and anxiety.
According to their findings, the combination of chemo plus endocrine therapy created more cancer-related cognitive impairment than endocrine therapy alone in both pre- and post-menopausal patients, and the damage was sustained over 36 months. As with the neuropathy findings, researchers concluded that interventions to prevent or treat cognitive impairment are needed to improve long-term quality of life for patients.
RxPONDER data was also used for an exploratory analysis of anxiety and fatigue in estrogen-receptor positive, HER2 negative (ER+/HER2-) breast cancer patients. Patients were randomized to either endocrine therapy alone or chemotherapy followed by endocrine therapy, and given baseline surveys to determine their anxiety and fatigue levels at the start of the study and again after 6, 12 and 36 months.
Results showed chemotherapy plus endocrine therapy produced significant fatigue scores compared to endocrine therapy alone in both pre- and post-menopausal patients. And while the fatigue scores improved over time, they did not return to baseline.
As for anxiety, patients had lower anxiety during treatment, compared to baseline, but the differences were not significant. Again, the researchers reiterated the need for therapeutic strategies to manage these treatment toxicities.
Black Wo(Men) Speak, a patient advocacy-led event held in conjunction with the San Antonio Breast Cancer Symposium, brought together advocates, oncologists, researchers and more to discuss how to improve diversity in clinical trials. Four organizations presented summaries of their research on Black and BIPOC participation in breast cancer clinical trials. Researchers can download the data from the event website: https://www.mbcalliance.org/black-women-speak/
Photo courtesy of Black Wo(Men) Speak
Investigating disparities in breast cancer
Cancer Consortium biostatistician Bill Barlow, PhD, acted as lead statistician on a SWOG study investigating race and clinical outcomes in the RxPONDER cohort. This large trial demonstrated the efficacy of a 21-gene recurrence score to determine if chemotherapy is necessary in early-stage breast cancer; since then, it’s become an important tool to guide treatment decisions.
But are all patients benefitting equally from it?
The investigators analyzed the clinical outcomes of participants by race and ethnicity to determine who achieved invasive disease-free survival. Out of a total of 4,048 women with ER+/HER2- breast cancer with limited lymph node involvement and a recurrence score under 25 (indicating no need for chemotherapy), the ethnicity breakdown was 70% white patients, 6.1% Black patients, 15.1% Hispanic patients, 8% Asian patients and .8% Native American/Pacific Islander patients, a percentage too low to include in the survival analysis.
Analysis showed that recurrence scores did not differ among the racial subgroups; additionally, there were no significant differences in tumor size or the number of positive lymph nodes. However, tumor grade (a measure that determines the aggressiveness of the cancer on a scale of 1 to 4) was significantly different among the groups.
Black and Hispanic women tended to have more grade 3 tumors (the higher the number, the more aggressive the cancer) than white or Asian women. In addition, the overall five-year invasive disease-free survival rate was lower for Black women than for others in the study.
“Black women with this type of breast cancer have worse outcomes compared to white women despite similar recurrence score results,” the investigators wrote. “There remains an important need for novel approaches to improve clinical outcomes, particularly for Black women.”
Led by Yara Abdou, MD of the University of North Carolina, who presented the findings at SABCS, the team found that disparities remained, even after adjusting for a number of factors.
“We continue to note worse outcomes for Black patients, suggesting race is independently prognostic,” she said.
Dr. Eric Winer, director of Yale Cancer Center and president-elect of the American Society of Clinical Oncology, commented “This is one of the most important presentations we’ll hear here,” at the end of the session.
‘Black women with this type of breast cancer have worse outcomes compared to white women despite similar recurrence score results. There remains an important need for novel approaches to improve clinical outcomes, particularly for Black women.’
— Findings from the Race and Clinical Outcomes in the RxPONDER Trial, presented at SABCS 2022
Who goes to the ER during treatment?
Lead author Dawn Hershman, MD, of Columbia University Medical Center in New York, and SWOG researchers, including Fred Hutch’s Unger and Barlow, also dug into data to see which elderly breast cancer patients had unplanned emergency room visits. Their retrospective analysis was presented during a spotlight poster discussion by Hershman during the conference.
The SWOG team set out to discover if insurance status might be a proxy for structural barriers to outpatient quality care, since many unplanned ER visits and hospitalizations are preventable. They first pooled breast cancer patients ages 65 and older who’d participated in SWOG clinical trials from 2001 to 2019, linking the trial data to the participants’ insurance claims (either Medicare alone, Medicare plus commercial insurance or Medicare plus Medicaid).
After examining just over a thousand patient records, they found patients with Medicare and Medicaid were much more likely to have an ER visit within 12 months of their clinical trial registration.
“Despite participation in a breast cancer clinical trial, patients with Medicare plus Medicaid had a two-fold increased risk of unplanned ER visits despite controlling for clinical, demographic and prognostic factors,” the team wrote in their analysis.
As Hershman explained in her presentation, the findings suggest that “access and structural factors may adversely influence unplanned emergency room visits for socioeconomically vulnerable old patients with breast cancer.”
In conjunction with reducing insurance-related barriers to clinical trials, she said efforts are needed to ensure adequate clinical resources for more vulnerable older patients in order to prevent unplanned use of acute care.
Dense breasts and elevated risk of cancer
Fred Hutch biostatistician and Rosalie and Harold Rea Brown Endowed Chair Ruth Etzioni, PhD, and researchers from three other institutions, shared data from a study regarding the association between dense breast tissue and breast cancer aimed at determining the true nature of this risk or whether it had been overstated.
“It’s well-known that women with dense breasts have a higher risk of breast cancer, but their process of diagnosis for them can be quite different than the process of women who don’t have dense breasts,” Etzioni said, explaining that women with dense breasts often have supplemental screening, such as ultrasound or MRI.
“We wanted to know the real risk because the more you look, the more you find,” she said. “Have we been looking so much more that we’ve exaggerated how high their risk is?”
The answer is no.
Etzioni and first author Jane Lange, PhD, from Oregon Health & Science University, used data from the Breast Cancer Surveillance Consortium, the leading collaborative network of U.S. breast imaging registries, to analyze mammogram and cancer outcomes in women aged 40 to 54 who had their first digital mammogram between the years 2000 and 2018. Out of a total of 33,542 women, 15,092 had non-dense breasts (meaning, they were almost entirely fatty or had scattered fibro glandular density). The remaining 18,450 had dense or extremely dense breasts.
After comparing the two groups, Etzioni said the data showed a robust increased risk of breast cancer among women with dense breasts.
“It’s a real increase in risk and not an artifact of the difference in what’s done to them,” she said. “It’s good for women to know if they have dense breasts. It’s an important piece of information to have in her health toolkit.”
A deeper dive into the new FES-PET imaging tracer
Fred Hutch physician-scientist Hannah Linden, MD, and colleagues presented a poster highlighting research on a new FDA-approved PET scan imaging tracer known as 18F-Fluoroestradiol or FES-PET. Linden and Specht also shared findings on both FES and the standard glucose-based (FDG) imaging tracers during a satellite symposium sponsored by the Society for Nuclear Medicine and Molecular Imaging.
FES-PET was recently approved for characterizing disease in patients with ER+ breast cancer. Linden and colleagues Natasha Hunter, MD, Specht and others, looked at its utility in patients with ER+, HER2+ and progesterone receptor positive tumors, often referred to as triple positive breast cancer. The team retrospectively examined results of both FES-PET and 18F -Fluorodeoxyglucose, or FDG-PET, (two different tracers) on more than 200 breast cancer patients, including both ductal and lobular subtypes.
Upon analysis, they found that the FDG and FES agents’ activity were similar in this group of ER+ breast cancer patients, regardless of HER2 status.
“This suggests that in many patients with so-called ‘triple-positive’ disease, endocrine therapy [which suppresses estrogen production] may offer a powerful primary rather than ancillary tool in select patients,” Linden and team wrote.
“FES imaging, combined with FDG, could help identify which patients might benefit from HER2+ and ER+ targeted therapy — without chemotherapy,” Linden said.
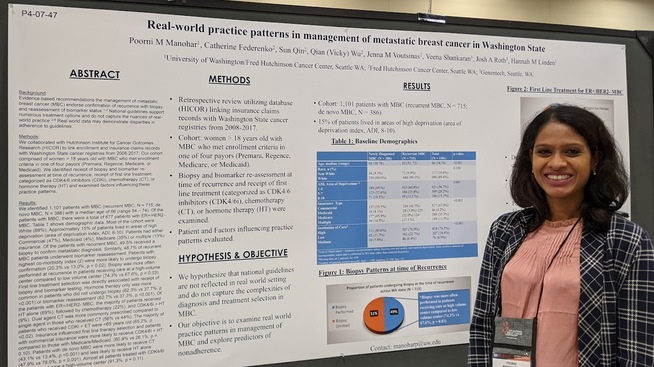
Fred Hutch breast cancer oncologist Dr. Poorni Manohar shared findings from a multi-site study in Washington state that showed that just half of breast cancer patients who recur with metastatic disease are receiving the recommended biopsies and biomarker tests. “People were surprised and concerned about the findings,” she said. Manohar has submitted a grant to test out clinical interventions to improve this.
Photo courtesy of Diane Mapes
Identifying gaps in metastatic cancer care
Fred Hutch breast cancer oncologist Poorni Manohar, MD, shared a poster on real-world practice patterns in the management of metastatic breast cancer in Washington state.
Although guidelines recommend that metastatic recurrence be confirmed with biopsy and a reassessment of biomarker status, Manohar and colleagues drilled down into the data to make sure patients were receiving this standard of care.
They analyzed the insurance coverage and the electronic health records of 1,101 patients with metastatic breast cancer, 386 of whom were diagnosed with de novo disease, i.e., metastatic from the very start as opposed to recurring later after treatment. Those whose disease had recurred totaled 715. The researchers then determined who among those 715 patients had — or hadn’t — received the recommended biopsies and biomarker tests.
“Of the patients with recurrent metastatic breast cancer, 49.5% received a biopsy to confirm the metastatic diagnosis,” Manohar reported. “Similarly, 48.7% of recurrent MBC patients underwent biomarker reassessment.”
In other words, half of the patients who should have received biopsies to confirm the molecular makeup of their new cancer in order to select the proper treatment, did not receive them.
Further analysis showed that biopsies that were performed were more often done at high-volume cancer centers compared to low-volume cancer centers. Additionally, patients with commercial insurance were more likely to receive the recommended treatment of CDK4/6 inhibitors plus endocrine therapy compared to those with Medicare or Medicaid. Similarly, CDK4/6 inhibitors were almost exclusively given to patients treated at the high-volume cancer centers.
“People were surprised and concerned about the findings,” she said. “It confirmed what I suspected may be occurring, but the degree of biopsy omission was higher than expected. It’s an important finding because it identifies a gap in our ability as a cancer community to offer the best resources to meet standard-of-care recommendations.”
And she has ideas on how to improve this.
“If we can increase access to resources, improve institutional experience with biopsy of challenging sites, and offer alternatives to biopsy, we could greatly enhance the quality of care for patients,” she said.
Patient advocacy efforts pay off
Health disparities and gaps in research were emphasized throughout SABCS 2022 and its related presentations, led in part by patient advocacy efforts.
The MBC Alliance presented a special Black Wo(Men) Speak Symposium on the night before the conference to emphasize the ongoing urgent need for diversity in clinical trials, as highlighted by survey data collected by MBC Alliance, TOUCH, the Black Breast Cancer Alliance, For the Breast of Us and Carrie’s TOUCH.
The final “Year in Review” session presenter Marleen Kok, MD, PhD, decried the lack of research — and SABCS’s lack of emphasis — on “unseen” lobular breast cancer, noting findings from a study done by an international group of lobular researchers including Fred Hutch’s Nancy Davidson, MD, Chris Li, MD, PhD, and others.
“There are still no reports on clinical trials specific for early ILC,” she said. “This is an unmet clinical need.”
And data on a new diagnostic scoring system was presented to help clinicians in the detection of another understudied (and often misdiagnosed) subtype, inflammatory breast cancer.